Brain tumors
Depending on the location, structure and degree of malignancy, brain tumor surgery often requires a multi-modal approach using various tactics, equipment and tools.
Microsurgical removal of brain tumors and the base of the skull is performed using:
A new generation microscope;
Neuronavigation systems for planning access and visual control of functionally important tracts and cortical zones around the tumor;
Neuromonitoring for intraoperative electropulse determination of functionally significant pathways and centers around the tumor;
Pre-endovascular embolization of tumor vessels to reduce the risk of blood loss during surgery;
Endoscopic equipment for monitoring and assistance;
Stereotactic biopsy for accurate and safe diagnosis;
A hybrid operating room for combining various surgical techniques.
The removed tumor is subjected to pathomorphological examination and molecular genetic analysis, a plan for further treatment, rehabilitation and follow-up is discussed and formed.

Diseases of the brain vessels
To turn off aneurysms, arteriovenous malformations and fistulas of the brain, our team performs both endovascular operations and microsurgical interventions, if necessary, with a combination of both techniques in a hybrid angiographic operating room.
Correction of hemodynamically significant stenoses of the internal carotid and vertebral arteries is performed by intravascular stenting.
In case of occlusion of the internal carotid, middle cerebral artery, Moya-moya disease, an extra intracranial bypass is performed.
After a certain period of time, all the operated patients undergo verification control endovascular and MRI studies.
Parkinson’s disease, tremor and dystonia
The team is continuously increasing its experience in the surgical treatment of motor disorders using a stereotactic system for deep brain stimulation.
Electrodes are inserted into certain areas (nuclei) of the brain, which are connected to a permanent subcutaneous stimulator.
After the operation, a special programming of the system is carried out to select the parameters of stimulation.



Epilepsy
“Epileptic Center” formed on the basis of the Hospital unites specialists of different profiles for effective pre-surgical selection of candidates and surgery.
Surgical treatment is indicated for pharmacoresistant epilepsy resistant to antiepileptic drugs.
The type of operation is due to the location of the epileptogenic focus and the form of epilepsy.
Very often, the epileptogenic focus is located in the temporal lobe, so such an operation as a temporal lobectomy is often performed.
If in your case there is a multi-focal or other unresectable form of epilepsy, you may be offered vagal stimulation.
Sometimes invasive electroencephalography is used to determine the localization of an invisible epileptogenic focus.
Epilepsy associated with other causes (cortical dysplasia, cavernous malformation, DNET, ganglioglioma, posttraumatic, etc.) is considered relative to a specific case.


Trigeminal neuralgia
The team is guided by an algorithm for choosing a personalized optimal surgery in each case.
The patient is subjected to a questionnaire, an MRI is analyzed for the presence of a neurovascular conflict, one of the treatment methods is discussed and determined - microvascular decompression with Teflon, percutaneous radiofrequency thermocoagulation, trigeminal nerve blockade, selection of the type and dose of the drug.
Hemifacial spasm
To eliminate muscle contraction on one half of the face, we perform a highly effective standard micro-vascular decompression of the facial nerve with a retrosigmoid approach with a pre-surgical and postoperative assessment of the degree of spasm.
Hydrocephalus
The development of hydrocephalus can be based on various causes and mechanisms (hemorrhage, brain injury, meningitis, occlusion of the cerebrospinal tract, tumor, and spontaneous idiopathic normotensive). Taking into account the possible complications and consequences associated with shunt dependence and shunt dysfunction, a thorough analysis with an assessment of the dynamics of symptoms, MRI, CT, tap test is required to select the parameters of the shunt system. We usually perform ventriculoperitoneal or ventriculolumbar bypass surgery with a pre-installed or programmable valve.
Facial palsy
After surgery on removal of the brain tumor, or due to other reasons (injury, stroke) paralysis of the facial muscles may occur, due to damage to the facial nerve, the level and degree of damage is determined by electroneuromyography. In such a situation, under the condition of a small prescription of the lesion, a partial restoration of nerve function is possible with the help of a lingual-facial anastomosis operation.
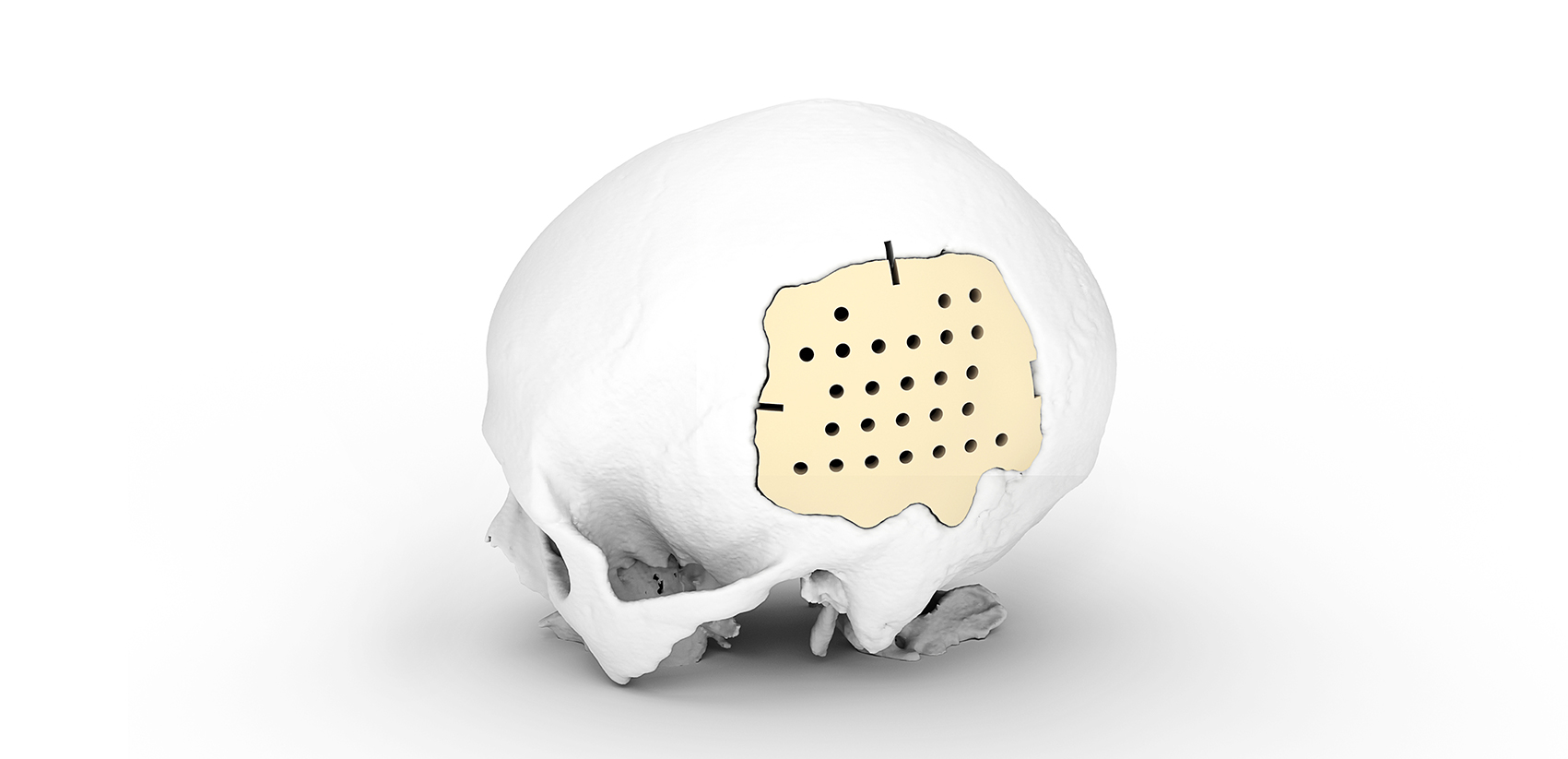
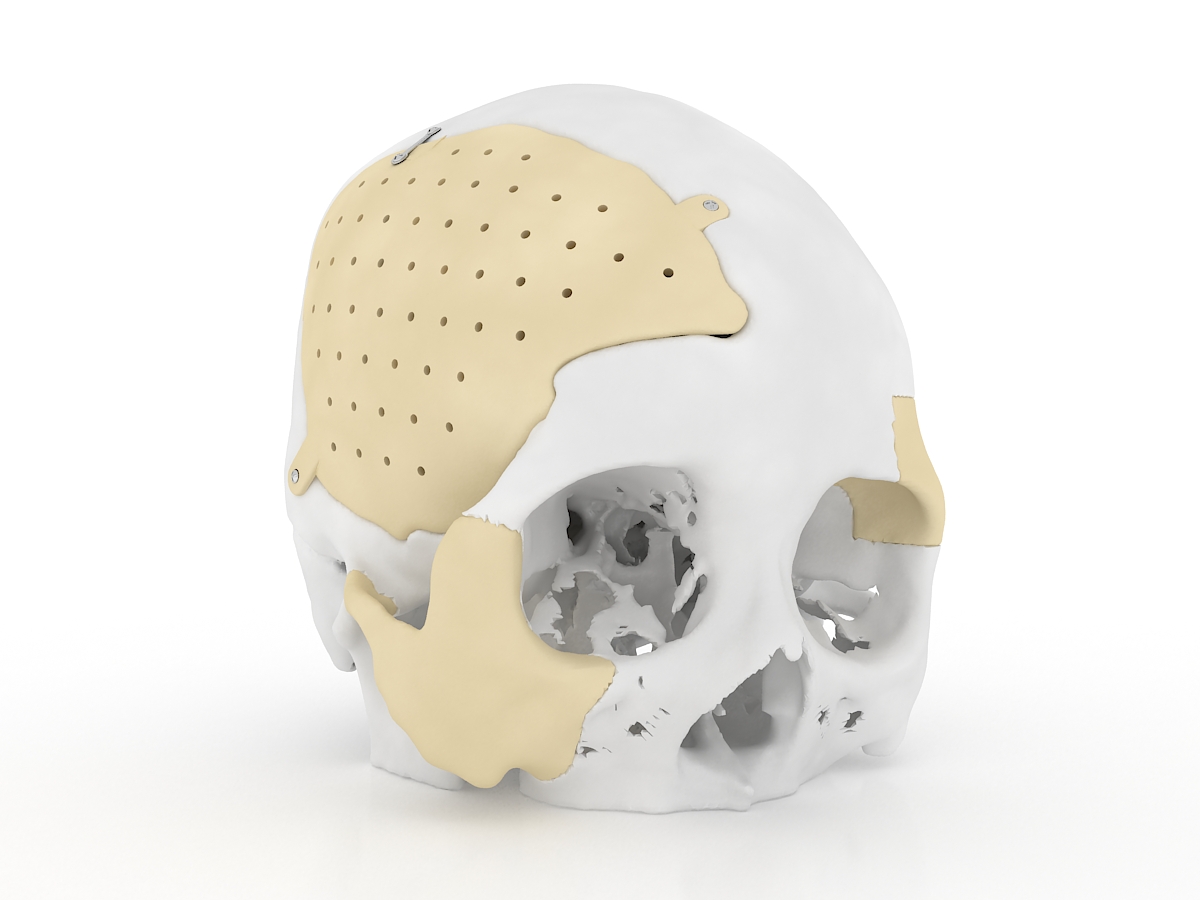
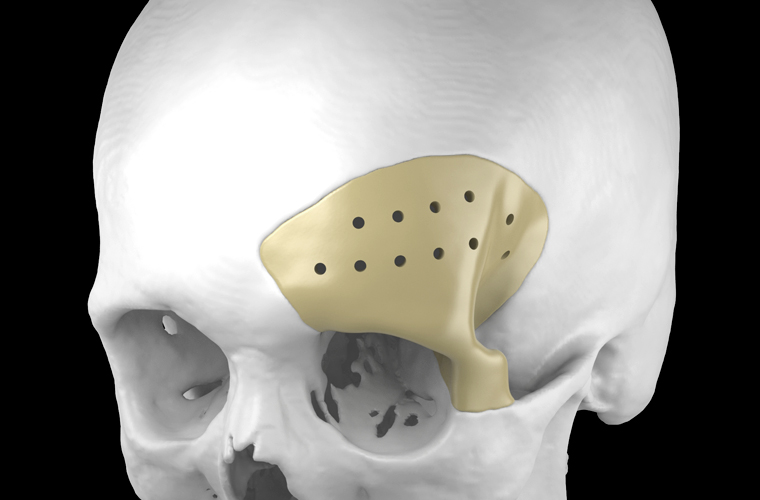
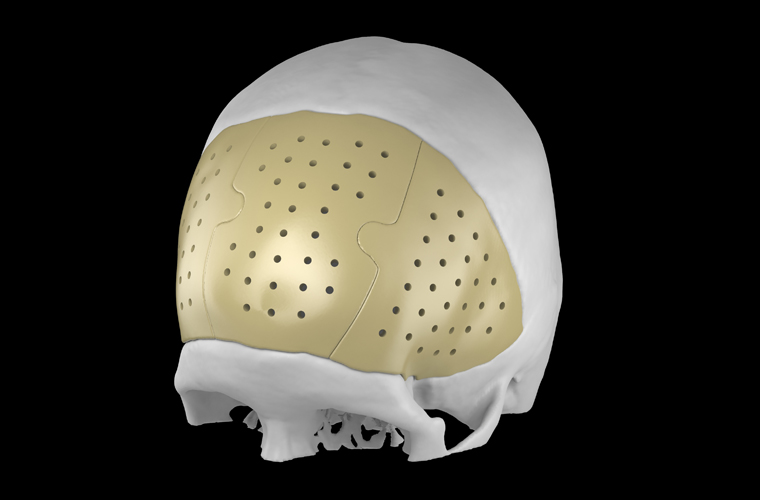
Intracranial hematomas, closure of skull defects
Subdural, epidural and intracerebral hematoma, brain contusion, depressed skull fracture are the consequences of traumatic brain injury, in which the operation to eliminate the compression of the brain is performed in an emergency or accelerated manner. The skull defect after trepanation can be closed with the use of various implants; three-dimensional individualized cranioplasty is also available.


Chiari Malformation and syringomyelia
In the presence of progressive symptoms (occipital headache, numbness and weakness in the arms and legs, dizziness, unstable gait, and others) of the disease, decompression of the posterior cranial fossa is performed, sometimes it is necessary to eliminate the fixed spinal cord syndrome by dissecting the terminal thread.
Neurosurgery of the spine, spinal cord and peripheral nerves
The team approach allows for dynamic development and effective implementation of high-tech interventions (microsurgery with neuromonitoring, stabilization with various metal structures, implantation of stimulants, nerve transfer) in the following conditions and diseases:
Herniated disc
Tumors of the spinal cord and spine
Spinal canal stenosis
Instability of the spine
Back pain
Lesions of peripheral nerves and plexuses